Review Article The interrelationship between Covid-19 and heart failure Panagiotis Theofilis1, Evangelos Oikonomou2, Dimitris Tousoulis1 1 1st Cardiology Department, General Hospital of Athens “Ippokrateio”, University of Athens Medical School 2 3rd Cardiology Department, General Hospital for Chest Diseases “Sotiria”, University of Athens Medical School Abstract Infections from the novel coronavirus (severe acute respiratory syndrome-Coronavirus 2, SARS-CoV2) and the associated disease (coronavirus disease 19, COVID-19) have heart failure (HF) as a risk factor and complication. As an independent predictor of poor prognosis, the presence of chronic HF may lead to increased morbidity and mortality in patients with COVID-19. This is achieved through multiple pathophysiologic mechanisms (inflammation, endothelial dysfunction, dysregulated coagulation), causing functional status deterioration in patients with chronic HF, combined with thrombotic and arrhythmic complications. De-novo HF in patients with COVID-19 is another frequent complication, often associated with right ventricular dysfunction. Beyond the acute manifestations of COVID-19, the long-term consequences of SARS-CoV-2 infection on the heart should not be neglected. Myocardial injury may be identified in a significant proportion of recovered individuals, with uncertain prognostic implications. Finally, vaccination against SARS-CoV2 is of great importance in patients with HF since it may lead to reduced morbidity and mortality. KeyWords: Covid-19 , heart failure Correspondence Address : Panagiotis Theofilis, 1st Cardiology Department, General Hospital of Athens, Ippokrateio”, University of Athens MedicalSchool, email: panos.theofilis@hotmail.com Introduction The emergence of the severe acute respiratory syndrome-Coronavirus 2 (SARS-CoV-2) with the associated disease (coronavirus disease 19, COVID-19) has led to a pandemic with increased morbidity and mortality, along with a significant worldwide healthcare burden. The main manifestation of COVID-19 includes pneumonia and acute respiratory distress syndrome. However, extrapulmonary manifestations are not uncommon, and are associated with disease severity and a poor prognosis. Additionally, many risk factors have been related to disease progression, such as heart failure (HF). The aim of this mini-review is to describe the importance of the interaction between HF and COVID-19. COVID-19 in heart failure patients Individuals with comorbidities are frequently faced with an increased risk of severe COVID-19 course and mortality, such as those with cardiovascular disease. In this particular patient subpopulation, mortality could even be 4-fold higher compared to the general population.1 More specifically, congestive HF is an independent prognostic factor of in-hospital mortality.2 Such patients have impaired immunity, are frail, and have limited ability to overcome the hemodynamic consequences of severe infections. It has been shown that, in HF patients, monocytes secrete pro- inflammatory cytokines compared to healthy individuals.3 When this is combined with the hyperinflammatory reaction to COVID-19, optimal cardiac function and cardiac output are required, which are not feasible in failing hearts. In patients with chronic HF, SARS-CoV-2 infection and COVID-19 can lead to acute decompensation of functional status, due to multiple mechanisms. Initially, the secretion of pro-inflammatory cytokines and the mobilization of macrophages and granulocytes leads to a cytokine storm that may exacerbate the preexisting injury.4-5 Endothelial dysfunction and generalized endotheliitis are cardinal features of COVID-19 pathophysiology, which can have detrimental consequences for patients with HF.6 The increased metabolic demands could potentially lead to cardiac dysfunction and either de novo HF or acute decompensation of chronic HF. At the same time, in septic conditions, coagulation abnormalities and platelet activation could have a hazardous effect. 5-7 The thrombotic complications of COVID-19 are well-known, and their non-negligible incidence may lead to the need for anticoagulation in hospitalized patients.8 Acute kidney injury represents an additional aggravating factor during COVID-19, which could promote volume overload and HF decompensation.9 Lastly, the use of various medications for COVID-19 management has been associated with proarrhythmic effects, such as QT interval prolongation, ventricular arrhythmogenesis, and sudden cardiac death. Patients with HF with a left ventricular assist device (LVAD) represent a unique subgroup, characterized by a different inflammatory profile with disrupted cellular immunity and a higher proinflammatory cytokine burden.10-11 However, there is no certain proof that this leads to an increased risk of SARS-CoV-2 infection. The optimal preload and afterload in such patients are critical in order to maintain cardiac output in infectious conditions. In case of hemodynamic abnormalities, many complications, such as right HF and device thrombosis, may ensue.12 Early case reports with coexisting COVID-19 and LVAD mentioned described the presence of persisting hypoxia and right heart failure, with multiorgan failure as the end result (13). The management of such patients should include their placement in a prone position, along with optimal medical therapy. Heart failure as a COVID-19 manifestation Among patients hospitalized for COVID-19, the incidence of de novo HF may reach 33% in patients who required admission to an intensive care unit (14). In a Spanish cohort of 3080 patients hospitalized for COVID- 19, the incidence of acute HF was 2.5%, and its development was associated with high rates of mortality that approached 50%. It should be stressed that 78% of patients with acute HF did not have a history of chronic HF.15 Pathophysiologic mechanisms such as inflammation and thrombosis are able to promote the development of HF. Beyond those, the activation of the sympathetic nervous system, along with SARS-CoV-2- induced myocardial damage and myocarditis are equally important in cardiac dysfunction development. Right ventricular dysfunction is a common phenomenon in COVID-19 due to the close relationship between the right ventricle and pulmonary circulation. Therefore, right HF contributes to swift hemodynamic destabilization, the incidence of arrhythmias and sudden cardiac death. Right ventricular dilatation is a frequent finding in autopsy studies of patients with severe COVID-19.16 Subsequently, echocardiographic studies identified a significant proportion of right ventricular dilatation (12-15%) and dysfunction (16-35%), along with increased pulmonary artery systolic pressure, even in subjects without known cardiac disease.17-19 Right ventricular remodeling in such patients was associated with a 2-fold increase in mortality. Furthermore, many patients with severe COVID-19 require positive pressure ventilation, which affects preload, afterload, and ventricular coupling, negatively impacting right ventricular function. 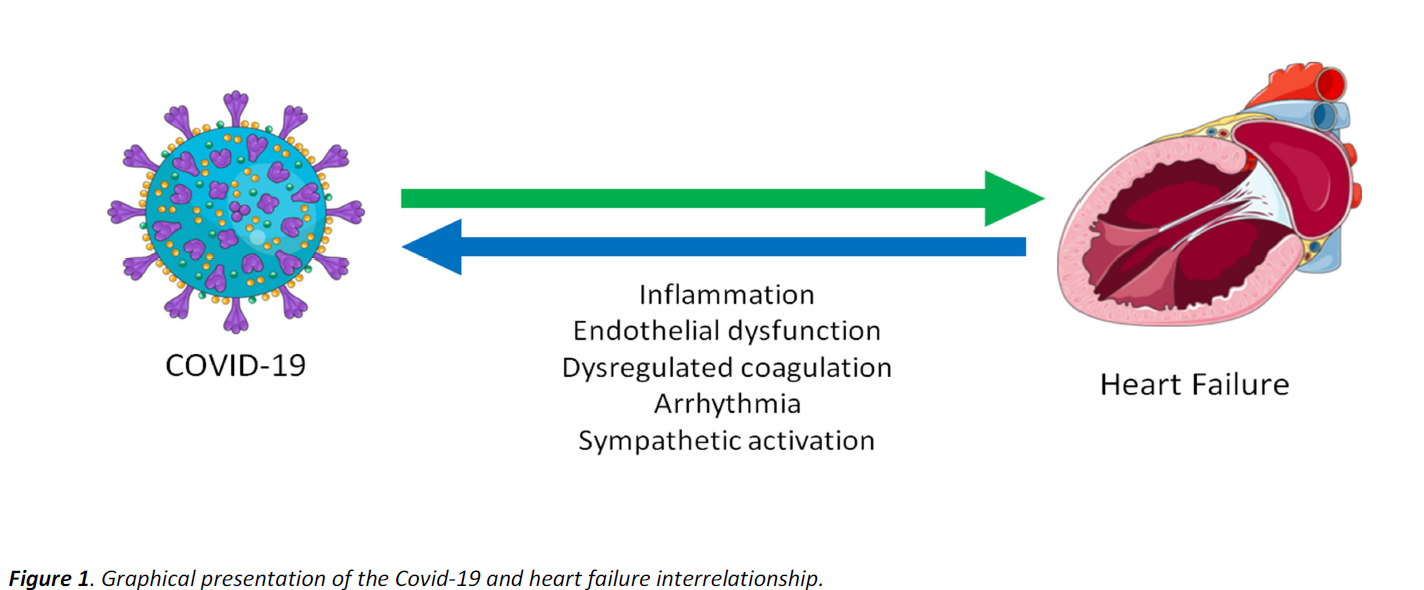
Long-term cardiac consequences of COVID-19 The long-term influence of SARS-CoV-2 and COVID-19 in various organ systems is a matter of extensive scientific investigation, since patients report persistent symptoms such as fatigue, dyspnea, and palpitations several months after the acute phase of the disease.20 Concerning cardiac complications, subacute myocarditis and prolonged inflammation are factors that aid HF development.21 Furthermore, endothelial dysfunction may be evident months after SARS-CoV-2 infection.6 In this context, the use of cardiac magnetic resonance imaging can provide useful data regarding the presence and the degree of injury, even in patients with mild symptoms during the acute phase of COVID-19. According to study results, it appears that cardiac involvement two months after the infection is evident in a significant proportion of patients, especially those with persisting symptomology.22 In a study of athletes after COVID-19, persisting myocarditis was noted in 15% and previous myocardial injury in 31%.23 The echocardiography study is also useful, as it can reveal the presence of diastolic dysfunction, abnormal left ventricular myocardial deformation, and pericardial effusion.24-26 The importance of those findings has not been explored, however. Nonetheless, it should be stated that persistent myocardial injury and ensuing fibrosis are independent factors for chronic HF development.27 Therefore, prompt recognition and continuous follow-up of those patients, along with the initiation of cardioprotective medication (renin- angiotensin-aldosterone system blockers, sodium- glucose cotransporter 2 inhibitors) may lead to positive outcomes. Management of patients with heart failure during the COVID-19 pandemic The implementation of social distancing measures and the prohibition of movements could indirectly affect patients with chronic HF.28 The limited accessibility to healthcare facilities and the fear of contracting SARSCoV- 2 infection are deterring factors for patients with HF regarding the programmed follow-up visits. The lack of close surveillance may have deleterious consequences on their prognosis. Therefore, informing HF patients about the need for frequent medical evaluation, including visits to specialized centers, is warranted even during the pandemic. not essential, and the patients should strictly follow preventive strategies (hand hygiene, wearing a face mask, and keeping their distance).30 Vaccination against SARS-CoV-2 should be performed in immune- compromised patients, such as those after heart transplantation, despite the uncertain immune response.35. Those patients, apart from the meticulous compliance with the preventive strategies mentioned above, may benefit from additional vaccine doses. The establishment of remote monitoring may be an acceptable alternative, since a greater attendance could be achieved, without increasing the rates of hospitalization or mortality. Despite the fact that a thorough clinical examination cannot be conducted remotely, the detection of certain features of congestion (lower limb edema, jugular vein distention) in conjunction with registration of body weight and vital signs could adequately guide the attending physician toward the optimal management of the patient. Remote pulmonary artery pressure monitoring is another alternative for the physicians of patients with HF. The management of those patients according to this parameter has led to significantly lower rates of hospitalization for chronic HF decompensation due to the constant optimization of medical therapy.29. SARS-CoV-2 vaccination in heart failure patients As previously mentioned, the presence of HF, especially in the elderly or frail individuals, is a potent risk factor for poor prognosis in COVID-19, leading to multiple complications and the need for intensive care unit admission with mechanical support of respiratory and cardiac function. On this basis, vaccination against SARS-CoV-2 in patients with HF is indicated, similarly to influenza and pneumococcal vaccination.30 Large clinical studies of vaccines against SARS-CoV-2 included patients with HF and confirmed their efficacy and safety in this patient population.31-34 Vaccination should be conducted imminently, ideally in a stable, compensated HF state.30. Iron replenishment in cases of coexisting iron deficiency could potentially improve the vaccine’s efficacy.30 Following vaccination, the measurement of antibodies is not essential, and the patients should strictly follow preventive strategies (hand hygiene, wearing a face mask, and keeping their distance).30 Vaccination against SARS-CoV-2 should be performed in immunecompromised patients, such as those after heart transplantation, despite the uncertain immune response.35. Those patients, apart from the meticulous compliance with the preventive strategies mentioned above, may benefit from additional vaccine doses. Attending physicians should be aware of the rare complications such as thromboembolism and myocarditis, without however discouraging vaccination of HF patients for this reason.30 The development of local hematomas is another complication which more commonly affects subjects with thrombocytopenia or on antithrombotic treatment.30 However, a serious allergic reaction to vaccine components remains the only contraindication to vaccination, whose prevalence is not more common in patients with HF.36 Conclusion The presence of chronic heart failure is an independent indicator of poor prognosis in patients with COVID-19, as shown by the high morbidity and mortality rates in this subgroup. Through multiple pathophysiologic mechanisms, COVID-19 could lead to acute decompensation of chronic HF, along with thrombotic and arrhythmic complications. A de novo heart failure development in COVID-19 patients is frequently observed, and depends on right ventricular dysfunction. Long-term cardiac consequences of SARS-CoV-2 are of considerable clinical and scientific interest, as they are noted in a significant proportion of convalescent patients. At the same time, since patients with heart failure are in need of frequent monitoring, the implementation of social distancing measures could have detrimental effects on their prognosis, warranting the need for remote monitoring. Finally, vaccination against SARS-CoV-2 is vital in patients with heart failure, as it can lead to reduced morbidity and mortality rates. References 1. Parohan M, Yaghoubi S, Seraji A, Javanbakht MH, Sarraf P, Djalali M. Risk factors for mortality in patients with Coronavirus disease 2019 (COVID-19) infection: a systematic review and meta-analysis of observational studies. Aging Male. 2020;23(5):1416-24. 2. Consortium C-CC, Group LS. Clinical presentation, disease course, and outcome of COVID-19 in hospitalized patients with and without pre-existing cardiac disease: a cohort study across 18 countries. Eur Heart J. 2022;43(11):1104-20. 3. Ng TM, Toews ML. Impaired norepinephrine regulation of monocyte inflammatory cytokine balance in heart failure. World J Cardiol. 2016;8(10):584-9. 4. Sagris M, Theofilis P, Antonopoulos AS, Tsioufis C, Oikonomou E, Antoniades C, et al. Inflammatory Mechanisms in COVID-19 and Atherosclerosis: Current Pharmaceutical Perspectives. Int J Mol Sci. 2021;22(12). 5. Theofilis P, Sagris M, Antonopoulos AS, Oikonomou E, Tsioufis C, Tousoulis D. Inflammatory Mediators of Platelet Activation: Focus on Atherosclerosis and COVID- 19. Int J Mol Sci. 2021;22(20):11170. 6. Oikonomou E, Souvaliotis N, Lampsas S, Siasos G, Poulakou G, Theofilis P, et al. Endothelial dysfunction in acute and long standing COVID-19: A prospective cohort study. Vascul Pharmacol. 2022;144:106975. 7. Avila J, Long B, Holladay D, Gottlieb M. Thrombotic complications of COVID-19. Am J Emerg Med. 2021;39:213-8. 8. Farkouh ME, Stone GW, Lala A, Bagiella E, Moreno PR, Nadkarni GN, et al. Anticoagulation in Patients With COVID-19: JACC Review Topic of the Week. J Am Coll Cardiol. 2022;79(9):917-28. 9. Glowacka M, Lipka S, Mlynarska E, Franczyk B, Rysz J. Acute Kidney Injury in COVID-19. Int J Mol Sci. 2021;22(15). 10. Kimball PM, Flattery M, McDougan F, Kasirajan V. Cellular immunity impaired among patients on left ventricular assist device for 6 months. Ann Thorac Surg. 2008;85(5):1656-61. 11. Radley G, Pieper IL, Ali S, Bhatti F, Thornton CA. The Inflammatory Response to Ventricular Assist Devices. Front Immunol. 2018;9:2651. 12. Kilic A, Acker MA, Atluri P. Dealing with surgical left ventricular assist device complications. J Thorac Dis. 2015;7(12):2158-64. 13. Chau VQ, Oliveros E, Mahmood K, Singhvi A, Lala A, Moss N, et al. The Imperfect Cytokine Storm: Severe COVID-19 With ARDS in a Patient on Durable LVAD Support. JACC Case Rep. 2020;2(9):1315-20. 14. Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, et al. Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State. JAMA. 2020;323(16):1612-4. 15. Alvarez-Garcia J, Jaladanki S, Rivas-Lasarte M, Cagliostro M, Gupta A, Joshi A, et al. New Heart Failure Diagnoses Among Patients Hospitalized for COVID-19. J Am Coll Cardiol. 2021;77(17):2260-2. 16. Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy Brown J, Vander Heide RS. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med. 2020;8(7):681-6. 17. Dweck MR, Bularga A, Hahn RT, Bing R, Lee KK, Chapman AR, et al. Global evaluation of echocardiography in patients with COVID-19. Eur Heart J Cardiovasc Imaging. 2020;21(9):949-58. 18. Kim J, Volodarskiy A, Sultana R, Pollie MP, Yum B, Nambiar L, et al. Prognostic Utility of Right Ventricular Remodeling Over Conventional Risk Stratification in Patients With COVID-19. J Am Coll Cardiol. 2020;76(17):1965-77. 19. Szekely Y, Lichter Y, Taieb P, Banai A, Hochstadt A, Merdler I, et al. Spectrum of Cardiac Manifestations in COVID-19: A Systematic Echocardiographic Study. Circulation. 2020;142(4):342-53. 20. Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397(10270):220-32. 21. Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022;28(3):583-90. 22. Parwani P, Ordovas KG. Beyond the AJR: "Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19)". AJR Am J Roentgenol. 2021;217(1):260. 23. Rajpal S, Tong MS, Borchers J, Zareba KM, Obarski TP, Simonetti OP, et al. Cardiovascular Magnetic Resonance Findings in Competitive Athletes Recovering From COVID-19 Infection. JAMA Cardiol. 2021;6(1):116-8. 24. Brito D, Meester S, Yanamala N, Patel HB, Balcik BJ, Casaclang-Verzosa G, et al. High Prevalence of Pericardial Involvement in College Student Athletes Recovering From COVID-19. JACC Cardiovasc Imaging. 2021;14(3):541-55. 25. Ozer S, Candan L, Ozyildiz AG, Turan OE. Evaluation of left ventricular global functions with speckle tracking echocardiography in patients recovered from COVID-19. Int J Cardiovasc Imaging. 2021;37(7):2227-33. 26. Weckbach LT, Curta A, Bieber S, Kraechan A, Brado J, Hellmuth JC, et al. Myocardial Inflammation and Dysfunction in COVID-19-Associated Myocardial Injury. Circ Cardiovasc Imaging. 2021;14(1):e012220. 27. Zaccone G, Tomasoni D, Italia L, Lombardi CM, Metra M. Myocardial Involvement in COVID-19: an Interaction Between Comorbidities and Heart Failure with Preserved Ejection Fraction. A Further Indication of the Role of Inflammation. Curr Heart Fail Rep. 2021;18(3):99-106. 28. Oikonomou E, Aznaouridis K, Barbetseas J, Charalambous G, Gastouniotis I, Fotopoulos V, et al. Hospital attendance and admission trends for cardiac diseases during the COVID-19 outbreak and lockdown in Greece. Public Health. 2020;187:115-9. 29. Abraham WT, Adamson PB, Bourge RC, Aaron MF, Costanzo MR, Stevenson LW, et al. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. Lancet. 2011;377(9766):658-66. 30. Rosano G, Jankowska EA, Ray R, Metra M, Abdelhamid M, Adamopoulos S, et al. COVID-19 vaccination in patients with heart failure: a position paper of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2021;23(11):1806-18. 31. Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N Engl J Med. 2021;384(5):403-16. 32. Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med. 2020;383(27):2603-15. 33. Ramasamy MN, Minassian AM, Ewer KJ, Flaxman AL, Folegatti PM, Owens DR, et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet. 2021;396(10267):1979-93. 34. Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397(10269):99-111. 35. Itzhaki Ben Zadok O, Shaul AA, Ben-Avraham B, Yaari V, Ben Zvi H, Shostak Y, et al. Immunogenicity of the BNT162b2 mRNA vaccine in heart transplant recipients - a prospective cohort study. Eur J Heart Fail. 2021;23(9):1555-9. 36. Banerji A, Wickner PG, Saff R, Stone CA, Jr., Robinson LB, Long AA, et al. mRNA Vaccines to Prevent COVID-19 Disease and Reported Allergic Reactions: Current Evidence and Suggested Approach. J Allergy Clin Immunol Pract. 2021;9(4):1423-37.
visibility_offDisable flashes
titleMark headings
settingsBackground Color
zoom_outZoom out
zoom_inZoom in
remove_circle_outlineDecrease font
add_circle_outlineIncrease font
spellcheckReadable font
brightness_highBright contrast
brightness_lowDark contrast
format_underlinedUnderline links
font_downloadMark links