Nikakis Christos, MD1, Vasilopoulou Anastasia, MD, Msc, Apostolopoulos Alexandros P., Msc, PhD, Trichonas Antonios, MD1, Georgiou Flourentzos, MD1, Siderakis Emmanouil, MD1, Panagiotakis Ioannis, MD1, Stathopoulos Konstantinos, MD, PhD2, Chronopoulos Efstathios 2
1Trauma and Orthopaedic Department, Korgialeneio Benakeio Hellenic Red Cross Hospital, Athens, Greece.
2Research Laboratory of Musculoskeletal Diseases, University of Athens, KAT Hospital
Correspondence Address: Alexandros Apostolopoulos, email: aalexgr2000@yahoo.com
doi: 10.5281/zenodo.17108033.
The perioperative rate of blood transfusion in patients undergoing hip fracture surgery remains high. The use of tranexamic acid in hip surgery is found to decrease blood loss and transfusion rates.
A prospective study was conducted from November 2018 to January 2022 and included patients with hip fractures that underwent hip surgery in a Major Trauma Centre. A tranexamic acid(TXA) administration control protocol was established, and patients were randomly assigned in two groups with equal number of patients: Group A included those who received TXA and Group B was the control group. Patient’s demographics, fracture type, blood transfusion demands during operation and post operatively, thromboembolic events, mean operative time, and mortality rates were recorded for each group.
Both groups included 50 patients. In Group A, 8% of patients needed transfusion with 1 unit of condensed red blood cells, while in group B 50% of patients needed transfusion. Blood loss was higher postoperatively in Group B.
The use of TXA in hip fracture surgery in Major Trauma Centers is effective, as it decreases transfusion demands and is a safe option without affecting the incidence of thrombotic events and mortality rates.
Keywords: tranexamic acid, hip fracture, Major Trauma Centre, hip surgery, blood loss
Introduction
Hip fractures in the elderly remain a serious public health factor around the globe, as they are associated with high morbidity rates and high mortality rates that reach up to 30% within the first-year post-injury(1, 2). These types of fractures require immediate surgical treatment, however past medical history, hidden blood loss due to the fracture and need for massive blood transfusions need to be taken into consideration(3, 4). Studies show that bleeding following a hip fracture and subsequent surgery may also contribute to postoperative morbidity and mortality(1, 5).Geriatric patients that already receive anticoagulants are at a further risk of an
even higher blood loss.Postoperative anaemia can trigger cardiac or renal symptoms especially in patients suffering from cardiac preconditions or renal dysfunction(2).
It is observed that the need for blood transfusion during or after hip fracture procedure fluctuates from 20% to 60% (1, 3, 6). Allogenic blood transfusion is an important tool to correct anaemia, however, is associated with adverse effects, such as infectious diseases, haemolytic reaction, cardiovascular dysfunction, postoperative infection and is also found to increase hospital length of stay(2, 3).
Recent retrospective studies and meta-analyses indicate that the use of tranexamic acid in hip surgery significantly decreases blood loss and transfusion rates(1, 7-10). Tranexamic acid is a synthetic analog of the amino acid lysine. It serves as an antifibrinolytic by reversibly binding four to five lysine receptor sites on plasminogen. This decreases the conversion of plasminogen to plasmin, preventing fibrin degradation and preserving the framework of fibrin’s matrix structure(6, 11, 12).Tranexamic acid has roughly eight times the antifibrinolytic activity of an older analogue, ε-aminocaproic acid. It also directly inhibits the activity of plasmin with weak potency, and it can block the active site of urokinase plasminogen activator (uPA) with high specificity, one of the highest among all the serine proteases(6, 11, 12).
The purpose of this study is to present the effectiveness of the administration of tranexamic acid (TXA) (transamin) to patients suffering from hip fractures in a Major Trauma Centre evaluating the need for blood transfusions during their hospitalization and complication rates.
Materials and Methods
A prospective study was conducted from November 2023 to April 2025 and included patients with hip fractures that underwent hip surgery in a Major Trauma Centre.
A tranexamic acid administration control protocol was established for patients with hip fractures. Inclusion criteria included:intertrochanteric fractures and femoral neck fractures based on AO-OTA classification and Garden classification respectively, Hb preoperatively (Measurement of hemoglobin before the patient is admitted to the operating room), Hb postoperatively on the first and the third day, number of condensed red blood cells (pRBC), total blood loss preoperatively and postoperatively, thrombophlebitis, pulmonary embolism and first trimester mortality.
Exclusion criteria were presence of liver failure, renal failure, active coronary artery disease, presence of coronary stents as these patients already receive antiplatelet treatment and cannot be operated on immediately after admission, history of hemorrhagic stroke in the last year, anticoagulant treatment, coagulation disorders,
platelets < 50.000, surgery after the fifth day of admission to hospital.
Patients with hip fractures included in the study were randomly assigned in two separate groups as follows: 1) Group A included patients who were administered 1gr. tranexamicacid iv intraoperatively during skin incision and 1gr. tranexamic acid iv during wound closure 2) Group B included equal number of patients who were administered 1gr. Saline iv intraoperatively during skin incision and wound closure respectively.
Data regarding demographics of the patients, fracture type, blood transfusion demands during operation and post operatively, thromboembolic events, mean operative time, and mortality rates were recorded for each group separately.
All data were extracted using a Microsoft Excel spreadsheet. The study was not registered on Clinicaltrials.gov. The protocol for this study was approved by the Hospital Ethics Committee and all patients provided written informed consent.
Results
From the above-mentioned criteria, 100 patients with hip fractures were finally included in the study. Both groups included 50 patients. Regarding patient’s demographics, in group A, 66% (33/50) were females and 34% (17/50) were males. In group B, 58% (29/50) were females and 42% (21/50) were males. Mean age was 84 years (range, 75-94) in group A and 83 years (range, 72-89) in group B.
Fracture types in both groups are presented in table 1.
In Group A, 4 out of 50 patients (8%) needed to be transfused with 1 unit of condensed red blood cells,even though they were administered tranexamic acid (Table 2).No pulmonary embolism or thromboembolic event was observed. Mortality rates were 0 during the first trimester. Blood loss was of the order of 1-2 vials of RBC between the first and the third postoperative day.
Groups | Gender (number of patients) | Type of fracture (number of patients) | ||
Male | Female | Intertrochanteric | Femoral neck | |
A | N/A | 33 | 20 | 13 |
A | 17 | N/A | 10 | 7 |
B | N/A | 29 | 20 | 9 |
B | 21 | N/A | 12 | 9 |
Table 1. Patient’s demographics and fracture types | ||||
In Group B, 50% (25/50) of patients required transfusion with a unit of condensed red blood cells during the operative procedure (Table 2). Six percent (3/50) of patients developed pulmonary embolism. One patient died during the first trimester. Blood loss was of the order of 3-4 vials of RBC between the first and the third postoperative day.
Mean operative time was the same in both groups: 62 min.
Discussion
In this prospective study on TXA use in hipfracture surgery in a Major Trauma Centre, the authorsfound that the number of patients who required blood transfusion were significantly lower in Group A (TXA Group) compared to Group B.This is in accordance with the published literature, where TXA usage is found to beassociated with a17% decrease in blood transfusions(6, 13).Interestingly, in a case-control cohort study which was conducted among 271 patients undertaking hip hemiarthroplasty for intracapsular hip , the authors noted that a single preoperative dose of TXA reduced the chance of blood loss requirements by three times(14). This is also proper to findings from previous case series, which have shown a positive effect of TXA dosage on minimizing surgical blood loss and blood transfusions(14-16). This finding is highly important for public health systems, as allogeneic blood transfusion has been associated with longer hospital stays and higher costs , estimated at 1731$ per hospital admission and is also related to several complications mentioned above, while a single dose of tranexamic acid costs 5$ and has fewer reported complications(13, 17).
Interestingly, in Group A none of the patients developed DVT or PE. In another randomized controlled trial of 72 patients, Tengberg et al.(18)found that TXA reduced total blood loss by600 mL and reduced the risk of blood transfusion, without a notable increase in venousthromboembolic events at 90 days post surgically(18).These results have been found to be associated with another randomized clinicaltrial of 100 participants with intertrochanteric femur fractures who received2 doses of IV TXA – 1 dose given prior to surgery and 1 dose 3 h following surgery.The relative risk of blood transfusion was 0.5 within the TXA group and no thrombotic events were reported(19). However, recent meta- analysis shows that, there was no significant increase in VTE risk between patients in TXA groups and non TXA groups(6, 8, 20, 21).
It is worthy of mention that patients presented in this study had various types of hip fractures both intracapsular and extracapsularthat require different types of surgical interventions.The majority of fractures,however,in this study were extracapsular. In general, extracapsular hip fractures are connected with massive blood loss compared tointracapsularones. Taking that into consideration, the effect of TXA may range in different types of hip fractures, and thus in various surgical methods.
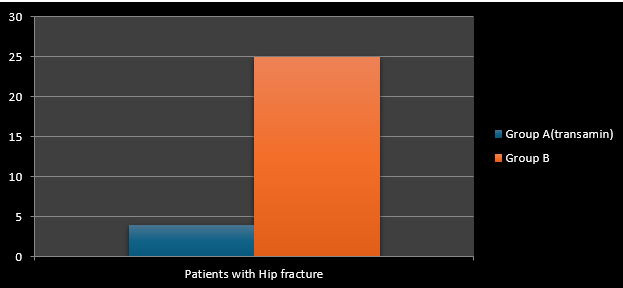 |
Table 2. Number of patients that required blood transfusion in both groups
|
The most common surgical treatment for extracapsular hip fractures is the use of an intramedullary nail. Intracapsular hip fractures are managed differently based on the extent of the fracture displacement(12). Percutaneous Pinning is an invasive surgical technique used to treat certain types of fractures including valgus impacted and non-displaced femoral neck fractures in younger patients, whereas displaced femoral neck fractures in older patients are often treated with hip hemiarthroplasty or total hip arthroplasty(12).
In this study complications and mortality rates did not differ significantly between the two groups. These findings are consistent with the literature, where thrombotic events, infections, ischemia, and mortality rates had no statistically significant differences between TXA groups and comparator groups(1, 20, 22, 23).
The ideal regional dosing of TXA to maximize efficacy whileminimizing the risks of potential side effects remains an active area of research. In this study, patients were administered one dose of TXA iv during skin incision and one during skin closure. Published studieshave been inconsistent regarding dosing regimens. Variousdosing regimens for TXA have been studied to establish the best results. Some protocols suggest a single dose before surgery, a preoperative dose followedby a second dose 3 hours later, while others recommend a preoperative dose followed by continuousintraoperative infusion, or a preoperative dose followed by a24-hour continuous infusion postoperatively. However, future studies should prioritize head-to-head comparisons of dosing strategies of TXA inhip fracture patients(6).
The optimal route of administration of TXA remains uncertain.In most studiespublished in the literature TXA is administered intravenously. TopicalTXA has also gained attention in recent medical literature. However, the available data on its long-term safety and efficiency of topical TXA compared to IV TXA are somewhat limited in hip fracture patients(6, 13). Emara et al. in a randomized control trial presented that both topical and IVTXA are equally effective at reducing bleeding and the need for blood transfusion however, IV TXAadministration was linked to a 30% increased risk of VTE events compared to topical TXA. Therefore, the authors of that study concludedthat theuse of topical TXA may be a safer choice compared to IV TXA(15).
Limitations
This study has several limitations. First, this is not a randomized controlled trial and there is not strong statistical evidence regarding the results presented. In addition, there is not a long term follow up period, as patients’ data were recorded up to the first trimester. The sample of the patients included in this study was relatively low compared to other studies.
Conclusion
In conclusion, the use of TXA in hip fracture surgery in Major Trauma Centers is highly effective, as it decreases transfusion demands and is a safe option without affecting the incidence of thrombotic events and mortality rates. Our results are consistent with other recently published studies in the literature, however more studies are needed to further assess the optimum route, dosage, and efficacy of TXA in patients with hip fractures.
References:
- Wilharm A, Wutschke I, Schenk P, Hofmann GO. Tranexamic Acid in Hip Hemiarthroplasty Surgery: A Retrospective Analysis of Perioperative Outcome. Geriatric Orthopaedic Surgery & Rehabilitation. 2023;14:21514593221147817.
- Zhou X-d, Zhang Y, Jiang L-f, Zhang J-j, Zhou D, Wu L-d, et al. Efficacy and Safety of Tranexamic Acid in Intertrochanteric Fractures: A Single-Blind Randomized Controlled Trial. Orthopaedic Surgery. 2019;11(4):635-42.
- Darren C, Graham E, Brian F, Brad S, Adrienne K, Yifun C, et al. Topical tranexamic acid in hip fractures: a randomized, placebo-controlled double-blinded study. Canadian Journal of Surgery. 2021;64(4):E449.
- Wilharm A, Wutschke I, Schenk P, Hofmann GO. Tranexamic Acid in Hip Hemiarthroplasty Surgery: A Retrospective Analysis of Perioperative Outcome. Geriatr Orthop Surg Rehabil. 2023;14:21514593221147817.
- Moran J, Kahan JB, Morris J, Joo PY, O’Connor MI. Tranexamic Acid Administration at Hospital Admission Decreases Transfusion Rates in Geriatric Hip Fracture Patients Undergoing Surgery. Geriatr Orthop Surg Rehabil. 2022;13:21514593221124414.
- Miangul S, Oluwaremi T, El Haddad J, Adra M, Pinnawala N, Nakanishi H, et al. Update on the efficacy and safety of intravenous tranexamic acid in hip fracture surgery: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2023;33(5):2179-90.
- Augustinus S, Mulders MAM, Gardenbroek TJ, Goslings JC. Tranexamic acid in hip hemiarthroplasty surgery: a systematic review and meta-analysis. Eur J Trauma Emerg Surg. 2023;49(3):1247-58.
- Baskaran D, Rahman S, Salmasi Y, Froghi S, Berber O, George M. Effect of tranexamic acid use on blood loss and thromboembolic risk in hip fracture surgery: systematic review and meta-analysis. HIP International. 2017;28(1):3-10.
- Bloom DA, Lin CC, Manzi JE, Mojica ES, Telgheder ZL, Chapman CB, et al. The Efficacy of Tranexamic Acid for the Treatment of Traumatic Hip Fractures: A Network Meta-Analysis. J Orthop Trauma. 2023;37(7):341-5.
- Tripathy SK, Varghese P, Kumarasamy AKN, Mishra NP, Neradi D, Jain M, et al. Safety and Efficacy of Tranexamic Acid in Hip Hemiarthroplasty for Fracture Neck Femur: a Systematic Review and Meta-analysis. Indian J Orthop. 2023;57(1):33-43.
- Fenwick A, Antonovska I, Pfann M, Mayr J, Wiedl A, Nuber S, et al. Does tranexamic acid reliably reduce blood loss in proximal femur fracture surgery? Eur J Trauma Emerg Surg. 2023;49(1):209-16.
- Ramirez RJ, Spinella PC, Bochicchio GV. Tranexamic Acid Update in Trauma. Crit Care Clin. 2017;33(1):85-99.
- Cheung ZB, Anthony SG, Forsh DA, Podolnick J, Zubizarreta N, Galatz LM, et al. Utilization, effectiveness, and safety of tranexamic acid use in hip fracture surgery: A population-based study. J Orthop. 2020;20:167-72.
- Lee C, Freeman R, Edmondson M, Rogers BA. The efficacy of tranexamic acid in hip hemiarthroplasty surgery: An observational cohort study. Injury. 2015;46(10):1978-82.
- Emara WM, Moez KK, Elkhouly AH. Topical versus intravenous tranexamic acid as a blood conservation intervention for reduction of post-operative bleeding in hemiarthroplasty. Anesth Essays Res. 2014;8(1):48-53.
- Sadeghi M, Mehr-Aein A. Does a single bolus dose of tranexamic acid reduce blood loss and transfusion requirements during hip fracture surgery? A prospective randomized double blind study in 67 patients. Acta Medica Iranica. 2007;45.
- Huynh PAN, Miller M, Will R. Intravenous Tranexamic Acid Decreases Blood Transfusions and Blood Loss for Patients with Surgically Treated Hip Fractures. Geriatric Orthopaedic Surgery & Rehabilitation. 2021;12:21514593211063668.
- Tengberg PT, Foss NB, Palm H, Kallemose T, Troelsen A. Tranexamic acid reduces blood loss in patients with extracapsular fractures of the hip: results of a randomised controlled trial. Bone Joint J. 2016;98-b(6):747-53.
- Stojadinovic IB, Ristic BM, Knezevic DR, Milenkovic ZS, Prodanovic NS, Zornic NR, et al. The effect of tranexamic acid on the reduction of intraoperative and postoperative blood loss and thromboembolic risk in patients with hip fracture. Open Med (Wars). 2022;17(1):857-62.
- Zhang P, He J, Fang Y, Chen P, Liang Y, Wang J. Efficacy and safety of intravenous tranexamic acid administration in patients undergoing hip fracture surgery for hemostasis: A meta-analysis. Medicine (Baltimore). 2017;96(21):e6940.
- Agius C, Cole E, Mifsud MG, Vasireddy A. The Use of Tranexamic Acid in Hip Fracture Surgery-A Systematic Review and Meta-analysis. J Orthop Trauma. 2022;36(12):e442-e8.
- Sahni G, Sood M, Girdhar D, Sahni P, Jain AK, Kumar S. To Analyze the Role of Intravenous Tranexamic Acid in Hip Fracture surgeries in Orthopedic Trauma. International Journal of Applied and Basic Medical Research. 2021;11(3):139-42.
- Zhang J, Fan X, Zheng Y, Wu J, Yuan X. Intravenous application of tranexamic acid in intramedullary nailing for the treatment of geriatric intertrochanteric fractures: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2023;24(1):614.
