Correspondece Address. Kotsiou Antonia, Microbiology Dpt. School of Medicine & Aretaieio University Hospital, National and Kapodistrian University of Athens, email: akotsiou@med.uoa.gr
Abstract
Aim: This review aims at investigating the diagnosis and treatment delays caused by the shift of health services towards corona virus pandemic management.
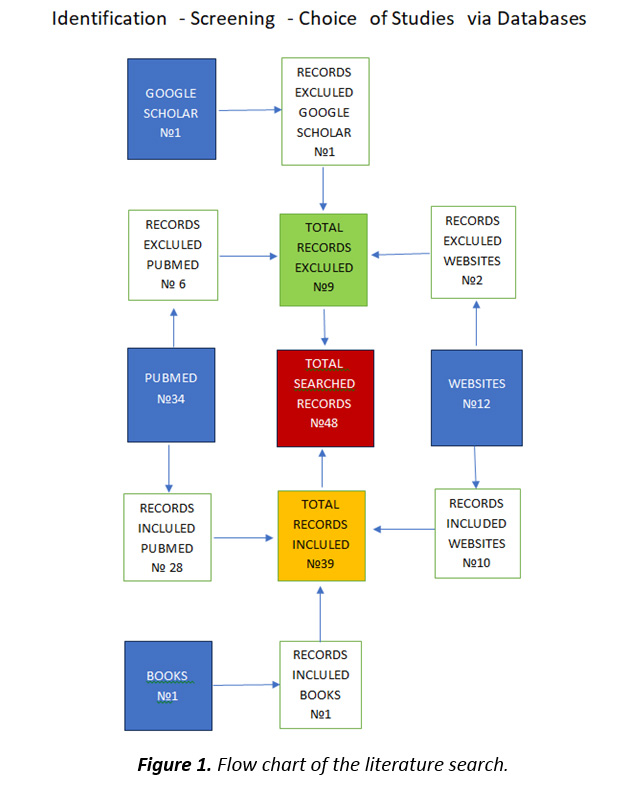
Methods: An extended literature search using reliable databases and the Terms: coronavirus disease, diagnostic delays, screenings, resulted in 48 relevant records. Out of them 9 were excluded and the remaining 39 were included in the study, 28 Pubmed, Websites10 and 1 Book.
Results: During pandemic, cancer screening programs, especially for the second deadliest colorectal cancer, have been decreased from 28 to 100% in different countries, endangering delayed diagnosis and poor treatment and survival outcomes. Delays were reported in care of patients with chronic limb-threatening ischemia and a higher major limb amputation rate (2.6% to 32.2%). Skin cancers biopsies decreased by 18% and 27% for non-melanoma and melanoma cases respectively. A substantial decrease in the number of cutaneous squamous cell carcinoma and basal cell carcinoma diagnoses ( -29% and -50% respectively), when compared to those expected from March to May 2020, was documented in a study, where the skin lesions behind the masks, kept on faces, remaining unnoticed. In the COVID-19 era, the national TB control program received less attention, leading to a worsening of the global TB epidemic. Additionally a new challenge for cholera control efforts in 2020 emerged, disrupting the hard-won years of progress against cholera in Africa, the continent bearing 54% of the global cholera burden. Moreover due to changes in routine health services, leprosy patients under multi- drug- therapy experienced drug shortages and limited access to medical care.
Conclusions: It is not an easy task to combine both preventive and emergency medicine under pandemic situation, but it deserves to try, by all means, to alleviate the potentially devastating consequences.
Keywords: coronavirus disease, diagnostic delays, screenings
Introduction
An increase in diagnostic and treatment delays for a range of medical conditions were observed during (COVID-19) pandemic. The Coronavirus disease 2019 (COVID-19), caused by an RNA virus SARS-COV2 (severe acute respiratory syndrome coronavirus), was declared a pandemic by the World Health Organization (WHO) on March 11, 2020. By May 22, 2021, 3,437,545 deaths had been registered by WHO, confirming the disease‘s severity. By the summer of 2022 official death toll from SARS-CoV-2 infection was approximately 6 million. [1]
Globally, the number of new cases decreases by 58% during the 28-day period of 8 January to 4 February 2024 as compared to the previous 28-day period, with over 503 000 new cases reported. The number of new deaths decreased by 31% as compared to the previous 28-day period, with over 10 000 new fatalities reported. As of 4 February 2024, over 774 million confirmed cases and more than seven million deaths have been reported globally. [2]
During COVID-19 lockdowns ( first from March to May 2020), healthcare systems had been challenged as they had to be focused on the care of patients with COVID-19, postponing many scheduled, especially preventive and non-urgent medical activities, for non-COVID patients. High risk individuals (patients and those with chronic diseases, at greater risk for complications from COVID-19) avoided themselves to visit healthcare services in fear of contracting the virus.
However all the other diseases did not vanish due to the emergence of corona virus and were not at all drawn away, instead they were neglected, endangering increased morbidity and mortality.
Materials and Methods
An extended literature search in English was conducted, using the MESH terms: coronavirus disease, diagnostic delays, and screenings. The chosen data bases were PubMed, Google Scholar and the websites of valid organizations such as the World Health Organization. A total of 48 relevant records were studied. After processing the literature, 39 publications were considered as pertinent to our key words search criteria, and finally included in the article. (Figure 1)
Figure 1. Flow chart of the literature search.
|
Results and Discussion
Cancer screening programs have been suspended in many countries, after the onset of the COVID-19 pandemic. Delays in diagnosis result in a more advanced stage of disease at presentation, requiring more complex care, higher costs and poorer response to both therapy and survival outcomes. [3, 4] Delays in any step may alter the outcome of the next step in the chain of cancer management. Interruptions in cancer screening led to reductions in the numbers of diagnosed cancer cases or their recurrence, ranging from 6% in Denmark to 52% in the United States. [5] Colorectal cancer is the third prevalent and second deadliest cancer in the world. So, early detection through screening is essential to reduce the mortality associated with this cancer. [6]
The decreased number of cancer screening programs has led to increased risk of a late diagnosis of colorectal cancer. [7, 8] In Italy, a decrease of more than 30% in colorectal cancer screening was observed between March 2020 and May 2021. [9] In the USA, a decrease in colonoscopies during 2020 was observed, especially among the population with a lower socioeconomic status. [10]
In general, colorectal cancer screening has decreased, from 28 to 100%, in different countries during pandemic period. Surveillance colonoscopy showed a decrease of 44.6 to 79%, prescription colonoscopy decreased 60 to 81%, and referrals to colonoscopy showed a 43% decline. However, emergency colonoscopy showed a 2 to 9% increase. The use of the fecal immunochemical test also declined although in specific areas used as a colonoscopy alternative. [11]
Treatment of colorectal cancer (surgery, chemotherapy, and long-term radiation therapy) has also decreased significantly or has been delayed, interrupted, or stopped. Only cases of emergency surgery and short-term radiotherapy increased. The waiting time for hospitalization and the length of hospital stay after surgery has been reported to be higher. Changes in patients’ treatment plans and complete to partial cessation of hospitals activities-that provided treatment services-were reported. [12]
In a study reviewing strategies employed, and limb salvage outcomes, during the COVID-19 pandemic, delays were reported in care, affecting major limb amputations in patients with chronic limb-threatening ischemia. A higher major limb amputation rate (2.6% to 32.2%) during the pandemic surge was reported in 5 of 6 publications. Four of 6 studies also reported minor amputations; 3 of these demonstrated an increase in minor amputations (7% to 17.7%). Further data are required to improve strategies for treating this population to minimize negative outcomes. [13]
The problem of diagnostic delay of skin cancers during the COVID-19 pandemic has been recognized by several studies. Canadian authors compared the number of biopsies for skin cancers during the first 15 weeks in 2020 and during the same period in 2019. They found a decrease in the number of biopsies for non-melanoma skin cancer and melanoma of 18% and 27%, respectively. A multicenter study, performed in northern-central Italy, showed that the number of skin cancer diagnoses fell by 56.7% in weeks 11 to 20 of 2020, compared with the average number noted in the same periods of 2018 and 2019 . Furthermore, a single-center retrospective study in Italy demonstrated that the number of advanced skin cancers, surgically treated between May 18 and November 18, 2020, was significantly higher than in the same period in 2019. [14- 16]
Slotman E et al 2022 investigated the impact of the COVID-19 pandemic on trends in diagnoses of keratinocyte carcinoma (cutaneous squamous cell carcinoma (cSCC) and basal cell carcinoma (BCC) in renal transplant recipients and the magnitude of diagnostic delays in The Netherlands. During the COVID-19 pandemic, due to diagnostic delays, the number of cSCC and BCC diagnoses substantially decreased when compared to the number of diagnoses expected from March to May 2020 (cSCC -29%, BCC -50%), across all age groups, both sexes, and all regions in The Netherlands. An additional reason for the diagnostic delay was the fact that, the skin lesions behind the mask remained unnoticed, since masks were kept on faces during most examinations. [17] Two renal transplant recipients developed skin cancers during the COVID-19 pandemic, and the tumors were diagnosed with a significant delay, after having postponed their medical visits and examinations for skin cancer screenings. Moreover, during clinical visits the patients were commonly asked to keep their protective masks on, increasing the risk of overlooking their facial skin changes
These were two women 66 and 67-year-old, having received renal allografts from deceased donors in 2010 and 2014 respectively and under tacrolimus, mycophenolate mofetil, and steroid maintenance. In June 2020 and January 2020 both noticed erosion at her left infraocular area the first and a reddish squamous lesion on her right cheek the second. Both patients did not inform their family physicians about their skin changes, because they avoided all non-nephrological medical visits during the pandemic and postponed the dermatologic examination, to avoid social contact as much as possible. Some months later they were both diagnosed with basal cell carcinoma the first and cutaneous squamous cell carcinoma the second. The additional reason for the diagnostic delay was the fact that they kept the masks on their faces during most examinations, with the skin lesions behind the mask consequently remaining unnoticed. [18]
During the pandemic, deaths attributed to cardiac events or strokes have increased more than deaths for any other non-COVID-19 diagnosis. [19, 20] Finlay et al 2023 examined the pandemic effects on health care systems and particularly the care deficits caused (or exacerbated) by health care delayed or foregone during the COVID-19 pandemic. These were deferred/delayed acute care for urgent conditions; the shift to virtual provision of outpatient care; shortages of drugs and devices and reduced access to diagnostic testing, cardiac rehabilitation, and homecare services. [21]
The same negative impact, of relocation of health services, was documented regarding the established and re- emerging infectious de diseases, potentially becoming more transmissible or more pathogenic. All-cause lower respiratory tract infection (LRTI) death in 2022 (57 per 100 000 children younger than 5 years) was 28% higher than in the pre-pandemic period. The higher incidence of all-cause LRTI admissions to hospital in 2022, compared with the pre-pandemic period, is partly due to ongoing COVID-19 admission to hospital and could worsen if other endemic respiratory pathogens revert to pre-pandemic incidence. [22]
In the COVID-19 era, the national TB control program received less attention, leading to a worsening of the global TB epidemic, though TB remains a major public health priority and is the second leading cause of mortality from infectious disease worldwide. TB, an ancient disease, remains one of the top 10 causes of human death. It is estimated that, approximately one quarter of the world’s population is infected with latent Mycobacterium tuberculosis. [23, 24]
The lower incidence of admission to hospital for pediatric tuberculosis is consistent with the lower rates of tuberculosis notification in South Africa during the COVID-19 pandemic. [25]
Maryam Koupaei et al 2021, in their systematic search included 20 case reports and 11case series on TB/COVID-19 co-infection published from January 1, 2019 to February 24, 2021, from 18 countries, the majority being from India (N = 6) and China (N = 4). A total of 146 patients (114 men and 32 women), co-infected with TB and COVID-19, were enrolled. The mortality rate was increased to 13.0% and the rate of discharged patients was 87.0%.Since TB, due to prolonged disease incubation time, is usually diagnosed later than COVID-19, the severity of the co-infection worsens. [26]
Finn McQuaid et al 2022, investigated if disruptions in TB services due to the COVID-19 pandemic, may have exacerbated inequalities in detection rates by age or sex. They compared trends in age- and sex- disaggregated case notifications for all forms of new and relapse TB, reported to the World Health Organization for 45 high TB burden countries from 2013 to 2019, to trend predicted notifications to observed notifications in 2020 to estimate the number of people with TB likely to have missed or delayed diagnosis. Some setting-specific inequalities had been observed, indicating that TB notification rates amidst COVID-19 pandemic were lower than expected for adults (with a similar rate for both men and women), whilst for children and the elderly notification rates were also lower than expected, that‘s to say, a large number of individuals are likely suffering from untreated TB disease directly as a result of the pandemic. [27]
The COVID-19 pandemic posed a new challenge for cholera control efforts in 2020, having disrupted the hard-won years of progress against cholera in Africa, bearing 54% of the global cholera burden. [28] It also led to a decrease in health workforce and control efforts to reform the healthcare system and promote universal access to safe drinking water, sanitation, and hygiene infrastructure. [29] It is worth remembering, that cholera was never fully eradicated and since 1817, seven cholera pandemics have spread from Asia to much of the world, the seventh still present, having begun in Yemen in October 2016 and still continuing to being currently the largest outbreak in the world, with 5000 new infections a day. [30, 31, 32]
Between 2015 and 2019, ten cholera outbreaks affected Sub-Saharan African countries: [33] The WHO and the Lebanese Ministry of Health announced on the 10 October 2022 the re-emergence of Cholera in Lebanon [34] As of December 19, 2021 and sudden increase in the number of cholera cases in April 2021 amidst COVID-19 pandemic, children aged 5 -14 appear to be hardest hit , the case fatality ratio reaching 3.3%, twice that associated with COVID-19.[ 35.]
In African countries with health care systems being overwhelmed by COVID-19, not only the fight against cholera was neglected, but moreover the pandemic negatively affected humanitarian programs to reduce cholera morbidity and mortality by 67% by the year 2023, targeting to eliminate cholera by 2030. [36]
Coronavirus disease 2019 has also limited the access of patients with Hansen’s disease to care, due to changes in routine health services. [37] Along with COVID-19 spread, there was a reduction in leprosy diagnosis in the general population and children under 15 years-old, and also an increase in multi bacillary cases diagnosed, signaling a serious impact of the pandemic on leprosy control strategies in Brazil. [38] The pandemic has therefore created a backlog of undiagnosed Hansen’s disease cases and a wave of delayed treatment initiation in Espírito Santo and across Brazil, equivalent to an entire years’ worth of cases (approximately 400 in the state and 28 000 nationally). [39]
In a study by Barbara de Barros et al 2021, it was documented that, the measures implemented to control transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2, in some areas led to medications shortages for leprosy, affecting individuals who need multidrug therapy (MDT) and long-term follow-up. Many patients were not able to travel to alternative referral centers, developed to counteract the negative impacts of the COVID-19 pandemic on leprosy diagnostic services, 80% percent reduced in endemic countries. [40]
The fight against COVID-19 pandemic became the center of the health systems worldwide, resulting in diagnostic delays and increased incidence of morbidity, according to the relevant literature from previous studies. Since large numbers of people are at particular risk of severe consequences from diagnosis and treatment delays, it is of great importance to implement policy options towards mitigating this risk. Clinicians, policymakers, and public health practitioners should be alert to the variety of presenting morbidity, from various agents during a pandemic, and not only from the pandemic itself.
Conclusions
When healthcare sources are turned away to cope with a devastating pandemic, challenges are raised by both old diseases re-emergence and neglected screening’s negative impact. The findings reveal that the Covid-19 has marked serious diagnosis and treatment delays in a wide range of health issues. Of course it is not an easy task to combine both preventive and emergency medicine. The critical point is to maintain such an attitude, as to be able to do one thing without neglecting the other.
The author declares that there is no conflict of interest
References
- World Health Organization WHO coronavirus (COVID-19) dashboard. Published June 13, 2022, Accessed June 14, 2022. https://covid19.who.int/
- COVID-19 epidemiological update – 16 February 2024 (who.int)
- Alkatout I, Biebl M, Momenimovahed Z, et al.. Has COVID-19 affected cancer screening programs? A systematic review. Front Oncol 2021; 11:675038 DOI: 10.3389/fonc.2021.675038
- Patt D, Gordan L, Diaz M, et al.. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform 2020; 4:1059–1071. DOI: 10.1200/CCI.20.00134
- Hamilton AC, Donnelly DW, Loughrey MB, et al.. Inequalities in the decline and recovery of pathological cancer diagnoses during the first six months of the COVID-19 pandemic: a population-based study. Br J Cancer 2021; 125:798–805. PMCID: PMC8245662 DOI: 10.1038/s41416-021-01472-0
- Lotfollahzadeh S, Recio-Boiles A, Cagir B. Colon Cancer.BookIn: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan.2023 Jun 3.PMID: 29262132Bookshelf ID: NBK470380
- Holland J, Cwintal M, Rigas G, et al. The impact of delaying colonoscopies during the COVID-19 pandemic on colorectal cancer detection and prevention. Surg Endosc. 2022; 15:1-10, DOI: 10.1007/s00464-022-09211-z
- Boyle JM, Kuryba A, Blake HA, et al.. The impact of the first peak of the COVID-19 pandemic on colorectal cancer services in England and Wales: a national survey. Colorectal Dis. 2021; 23(7):1733-1744. DOI: 10.1111/codi.15622
- Mantellini P, Falini P, Gorini G, et al. Rapporto sui ritardi accumulati dai programmi di screening Italiana in seguito alla pandemia da COVID 19: quarto rapporto al 31 Maggio 2021 [Report on the backlogged delays due to the COVID 19 pandemic. Fourth report at 31 May 2021], Published May 2021, Accessed June 14, 2022, https://www.osservatorionazionalescreening.it/sites/default/files/allegati/Report%20ripartenza%20IV.pdf
- Fedewa SA, Star J, Bandi P, et al. Changes in cancer screening in the US during the COVID-19 pandemic. JAMA Netw Open, 2022;5(6):e2215490. doi: 10.1001/jamanetworkopen.2022.15490
- Mazidimoradi A, Tiznobaik A, Salehiniya H, Impact of the COVID-19 Pandemic on Colorectal Cancer Screening: a Systematic Review J Gastrointest Cancer. 2022 Sep;53(3):730-744. doi: 10.1007/s12029-021-00679-x. Epub 2021 Aug 18.
- Mazidimoradi A, Hadavandsiri F, Zohre Momenimovahed Z, Salehiniya H. Impact of the COVID-19 Pandemic on Colorectal Cancer Diagnosis and Treatment: a Systematic Review J Gastrointest Cancer. 2023 Mar; 54(1):171-187. DOI: 10.1007/s12029-021-00752-5
- Miranda J, Chung J, Mills J. Influence of the COVID-19 pandemic on the management of chronic limb-threatening ischemia. Semin Vasc Surg. 2021 Sep; 34(3):89-95. doi: 10.1053/j.semvascsurg.2021.05.006. Epub 2021 Jul 16. DOI: 10.1053/j.semvascsurg.2021.05.006
- Šitum M, Filipović N, Buljan M. A reminder of skin cancer during the covid-19 pandemic, Acta Dermatovenerol Croat. 2021 Apr; 291(1):58 PMID: 34477068
- Gomolin T, Cline A, Handler MZ. The danger of neglecting melanoma during the COVID-19 pandemic, J Dermatolog Treat, 2020; 31(5): 444-445. DOI: 10.1080/09546634.2020.1762844
- Villani A, Fabbrocini G, Scalvenzi M.The reduction in the detection of melanoma during the coronavirus disease 2019 (COVID-19) pandemic in a melanoma center of South Italy. J. Dermatol Treat. 2022 May; 33(3):1778. DOI: 10.1080/09546634.2020.1818674
- Slotman E, Schreuder K, Nijsten TEC et al. The impact of the COVID‐19 pandemic on keratinocyte carcinoma in The Netherlands: trends in diagnoses and magnitude of diagnostic delays. J Eur Acad Dermatol Venereol 2022; 36 (5): 680–687. PMID: 35092107 DOI: 10.1111/jdv.17976
- Mokos M, Bašić-Jukić N, Diagnostic Delays for Non-melanoma Skin Cancers in Renal Transplant Recipients during the COVID-19 Pandemic: What is Hiding Behind the Mask? Acta Dermatovenerol Croat, 2021 Jul; 29(2):111-113.
- Statistics Canada. Leading Causes of Death, Total Population (Age Standardization Using 2011 Population), Available at: 10.25318/1310080101-eng Accessed July 18, 2022.
- Sidney S., Lee C., Liu J., Khan S.S., Lloyd-Jones D.M., Rana J.S. Age-adjusted mortality rates and age and risk-associated contributions to change in heart disease and stroke mortality, 2011-2019 and 2019-2020. JAMA Netw Open 2022;5 DOI: 10.1001/jamanetworkopen.2022.3872
- McAlister FA, Parikh H, Lee DS, Wijeysundera H, Health Care Implications of the COVID-19 Pandemic for the Cardiovascular Practitioner. Can J Cardiol . 2023 Jun; 39(6):716-725. DOI: 10.1016/j.cjca.2022.11.014
- Izu A, Nunes M, Solomon F, Baillie V, Erafin N, Verwey Cet al. All-cause and pathogen-specific lower respiratory tract infection hospital admissions in children younger than 5 years during the COVID-19 pandemic (2020-22) compared with the pre-pandemic period (2015-19) in South Africa: an observational study Lancet Infect Dis. 2023 May 1;S1473-3099(23)00200-1. doi: 10.1016/S1473-3099(23)00200-1.
- WHO. Global Tuberculosis Report (2021) (Accessed November 01, 2021).
- Oga-Omenka C, Tseja-Akinrin A, Boffa J, Heitkamp P, Pai M, Zarowsky C. Commentary: Lessons from the COVID-19 global health response to inform TB case finding Healthc (Amst). 2021 Jun; 9(2):100487. doi: 10.1016/j.hjdsi.2020.100487. Epub 2020 Oct 22.
- Lebina L, Dube M, Hlongwane K, et al. Trends in paediatric tuberculosis diagnoses in two South African hospitals early in the COVID-19 pandemic. S. Afr. Med. J. 2020; 110:1149–1150, DOI: 10.7196/SAMJ.2020.v110i12.15386
- Koupaei M, Naimi A, Moafi N, et al, Clinical Characteristics, Diagnosis, Treatment, and Mortality Rate of TB/COVID-19 Coinfectetd Patients: A Systematic Review Front Med (Lausanne). 2021 Dec 1; 8:740593. doi: 10.3389/fmed.2021.740593. eCollection 2021
- McQuaid CF, Henrion M, Burke R, MacPherson P, Nzawa-SokoR , Horton K, Inequalities in the impact of COVID-19-associated disruptions on tuberculosis diagnosis by age and sex in 45 high TB burden countries BMC Med. 2022 Nov 14;20(1):432. doi: 10.1186/s12916-022-02624-6.
- Uwishema O, Okereke M, Onyeaka H, Mehediasan M, Donatus D et al, Threats and outbreaks of cholera in Africa amidst COVID-19 pandemic: a double burden on Africa’s health systems.Trop Med Health. 2021 Nov 24; 49(1):93. doi: 10.1186/s41182-021-00376-2.
- The World Bank. Physicians (Per 1000 People)-Nigeria (2021): https://www.data. worldbank.org/indicator/SH.MED.PHYS.ZS?locations=NG
- Kuna A, Gajewsk M. Cholera – the new strike of an old foe. Int Marit Health 2017; 68(3):163-167. doi: 10.5603/IMH.2017.0029.
- Kaper C, Morris J, Levine M, Clin Microbiol Rev 1995 Jan; 8(1):48-86. doi: 10.1128/CMR.8.1.48
- World Health Organization (19 October 2022), Disease Outbreak News; Cholera – Lebanon. Available at: https://www.who.int/emergencies/ disease-outbreak-news/item/2022-DON416
- Centers for Disease Control and Prevention (CDC). Cholera – vibrio cholerae infection, Africa by Country, Atlanta (GA): CDC; 2021 [cited 2021 Apr 28]. Available from: https://www.cdc.gov/cholera/africa/locations.html Centers for Disease Control and Prevention (CDC) Cholera – vibrio cholerae infection. Africa by Country, Atlanta (GA): CDC; 2021
- World Health Organization (19 October 2022), Disease Outbreak News; Cholera – Lebanon. Available at: https://www.who.int/emergencies/ disease-outbreak-news/item/2022-DON416
- NCDCb. COVID-19 Nigeria (2021). Available from: Accessed https://www.covid19. ncdc.gov.ng January 10, 2022)
- James O. Global Task Force on Cholera Control: Use of Cholera Vaccine, Nigeria (2019). Available from: https://www.gtfcc.org/wp-content/uploads/2020/08/6th-gtfcc-working- group-on-ocv-meeting-2019-james-onah.pdf
- Marques NP, Teixeira Marques NC, Medeiros Cardozo I, Martelli D, et al . Impact of the coronavirus disease 2019 on the diagnoses of Hansen’s disease in Brazil, Rev Soc Bras Med Trop. 2021 Jul 23; 54: e02512021. doi: 10.1590/0037-8682-0251-2021. eCollection 2021.
- Silva da Paz W, Souza M, Dos Santos Tavares D, Ribeiro de Jesus A, et al . Impact of the COVID-19 pandemic on the diagnosis of leprosy in Brazil: An ecological and population-based study Lancet Reg Health Am. 2022 May; 9:100181. doi: 10.1016/j.lana.2021.100181. Epub 2022 Jan 15.
- Deps P, Collin SM, de Andrade V, Hansen’s disease case detection in Brazil: a backlog of undiagnosed cases due to COVID-19 pandemic. J Eur Acad Dermatol Venereol 2022 Oct; 36(10):e754 -e755 doi: 10.1111/jdv.18307 Epub 2022 Jun 14.
- de Barros B, Lambert SM, Negera E, et al . An assessment of the reported impact of the COVID-19 pandemic on leprosy services using an online survey of practitioners in leprosy referral centres. Trans R Soc Trop Med Hyg 2021 Dec 2; 115(12):1456-1461, doi: 10.1093/trstmh/trab084